Gut Health and Mental Well-being: New Research Unveils the Link

New research highlights a significant link between gut health and mental well-being, revealing how the gut microbiome influences brain function and mental health conditions like anxiety and depression.
Emerging scientific evidence increasingly points to the profound connection between our gut and our brain. This new research: the link between gut health and mental well-being sheds light on how maintaining a healthy gut can positively impact our mental state, offering potential new avenues for managing mental health.
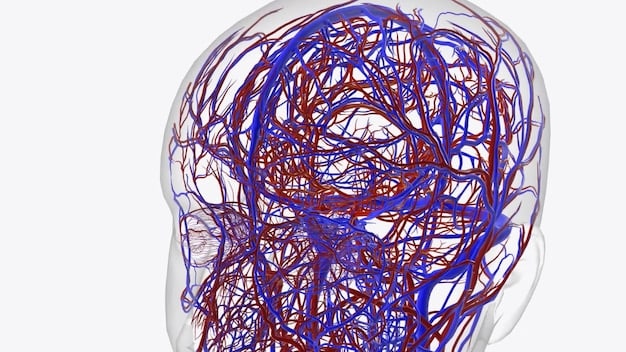
Understanding the Gut-Brain Axis
The gut-brain axis is a complex communication network that links the gut and the brain. This bidirectional pathway involves the nervous system, immune system, and endocrine system, allowing constant interaction between the gut microbiome and brain functions.
What is the Gut-Brain Axis?
The gut-brain axis refers to the communication network linking the gut and brain, a complex system influencing both physical and mental health
This intricate communication allows the gut to influence brain functions and mental states, and reciprocally, the brain can affect gut motility and secretion. This bidirectional influence highlights the importance of considering the gut microbiome in overall health.
Key Components of the Gut-Brain Axis
The composition and function of the gut microbiome play a crucial role in this axis. Gut bacteria produce neurotransmitters, short-chain fatty acids (SCFAs), and other metabolites that can affect brain function. An imbalance in the gut microbiome, known as dysbiosis, can disrupt this communication and contribute to mental health issues.
- Vagus Nerve: The highway for signals between the gut and the brain.
- Microbiota: Trillions of bacteria influencing mood, immunity, and digestion.
- Neurotransmitters: Serotonin, dopamine, and GABA produced in the gut to affect emotions.
The gut-brain axis isn’t just a one-way street; it’s a complex, bidirectional network that requires a balanced ecosystem for optimal function.
The Gut Microbiome and Mental Health
Recent research has uncovered specific ways in which the gut microbiome influences mental health. The gut microbiome produces various neurotransmitters and metabolites that directly impact brain function. Understanding this connection offers new possibilities for treating mental health conditions.
Neurotransmitters Produced in the Gut
The gut microbiome is responsible for producing a significant portion of the body’s neurotransmitters, including serotonin, dopamine, and GABA. These neurotransmitters play critical roles in regulating mood, anxiety, and overall mental well-being.
For example, approximately 90% of serotonin, a key neurotransmitter for mood regulation, is produced in the gut. By influencing the production of these neurotransmitters, the gut microbiome can have a profound impact on mental health.
How Gut Bacteria Affect the Brain
Specific gut bacteria can produce metabolites like SCFAs, which have anti-inflammatory and neuroprotective effects. These SCFAs can cross the blood-brain barrier and directly influence brain function, reducing inflammation and promoting neuronal health.
- Serotonin: Plays a pivotal role in mood regulation.
- Dopamine: Impacts reward and motivation.
- GABA: Helps reduce anxiety and promote relaxation.
Moreover, a healthy gut microbiome helps maintain the integrity of the gut lining, preventing the leakage of harmful substances into the bloodstream that can cause inflammation and affect brain function.
Research Findings: Gut Health and Mental Disorders
Several studies have explored the link between gut health and specific mental disorders. These findings provide insights into the potential for treating mental health conditions by targeting the gut microbiome. New research continues to reinforce these observations, offering more concrete data to prove this link.
Anxiety and the Gut Microbiome
Studies have shown that individuals with anxiety disorders often have altered gut microbiomes compared to healthy individuals. Specific gut bacteria that produce anti-inflammatory compounds may be reduced, while bacteria that promote inflammation may be increased.
Interventions such as probiotics and dietary changes aimed at improving gut health have been shown to reduce anxiety symptoms in some individuals.
Depression and Gut Health
Similarly, research has found a connection between gut health and depression. People with depression often have lower levels of certain beneficial gut bacteria and higher levels of harmful bacteria. The imbalance can affect neurotransmitter production and increase inflammation.
Clinical trials have explored the use of probiotics and prebiotics to improve gut health and alleviate depression symptoms. These interventions hold promise for adjunctive treatments for depression.
Strategies for Improving Gut Health
Improving gut health through dietary and lifestyle changes can positively impact mental well-being. These strategies can help promote a balanced gut microbiome and support the gut-brain axis.
Dietary Recommendations for Gut Health
A diet rich in fiber, fruits, and vegetables promotes a diverse and healthy gut microbiome. Fiber-rich foods, such as whole grains, legumes, and leafy greens, feed beneficial gut bacteria, promoting their growth and activity.
Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain probiotics, which introduce beneficial bacteria into the gut. Including these foods in your diet can help improve gut health.
Lifestyle Changes for Gut Health
Stress management is also crucial for gut health. Chronic stress can negatively impact the gut microbiome, leading to dysbiosis and inflammation. Practices like meditation, yoga, and deep breathing exercises can help reduce stress and support gut health.
- Probiotics: Introduce beneficial bacteria to the gut.
- Prebiotics: Feed existing good bacteria in the gut.
- Stress Management: Reduces negative impacts on gut health.
Regular exercise is another essential lifestyle factor. Physical activity can increase the diversity of the gut microbiome and promote overall health.
The Role of Probiotics and Prebiotics
Probiotics and prebiotics are two key players in supporting a healthy gut microbiome. Understanding how they work and incorporating them into your routine can contribute to improved mental well-being.
What are Probiotics?
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They are often referred to as good bacteria and can help restore balance to the gut microbiome.
Probiotics are available in supplement form and can also be found in fermented foods like yogurt and kefir. They can help replenish beneficial bacteria that may have been depleted due to diet, stress, or antibiotic use.
What are Prebiotics?
Prebiotics are non-digestible food ingredients that promote the growth and activity of beneficial gut bacteria. They serve as food for these bacteria, encouraging their proliferation and enhancing their beneficial effects.
Prebiotics are found in foods like garlic, onions, asparagus, bananas, and oats. They provide nourishment for the beneficial bacteria already present in the gut, helping them thrive and maintain a healthy gut ecosystem.
Future Directions in Gut Health and Mental Health Research
The field of gut health and mental health is rapidly evolving, with ongoing research exploring new potential treatments and interventions. These advancements offer optimism for individuals seeking to improve their mental well-being through gut health strategies.
Personalized Microbiome Interventions
Future research is likely to focus on personalized microbiome interventions tailored to individual gut microbiome profiles. By analyzing an individual’s gut microbiome composition, healthcare professionals can recommend specific probiotics, prebiotics, and dietary changes to address their unique needs.
This personalized approach holds great promise for optimizing the impact of gut health interventions on mental health outcomes.
Clinical Trials and Longitudinal Studies
More rigorous clinical trials and longitudinal studies are needed to further validate the link between gut health and mental health. These studies will provide more definitive evidence on the effectiveness of various gut health interventions for treating mental disorders.
Additionally, longitudinal studies can help researchers understand how changes in the gut microbiome over time influence mental health trajectories, paving the way for early interventions and preventative strategies.
| Key Point | Brief Description |
|---|---|
| 🧠 Gut-Brain Axis | Complex communication between gut and brain. |
| 🦠 Gut Microbiome | Produces neurotransmitters affecting mental health. |
| 🌱 Probiotics & Prebiotics | Support a healthy and balanced gut. |
| 🍎 Dietary Changes | Fiber-rich diet improves gut and mental health. |
Frequently Asked Questions
▼
The gut microbiome produces neurotransmitters like serotonin, which regulates mood. Imbalances in gut bacteria can disrupt neurotransmitter production, impacting mental health.
▼
Foods rich in fiber, such as fruits, vegetables, and whole grains, promote a diverse and healthy gut microbiome, supporting beneficial bacteria growth.
▼
Some studies suggest that probiotics can help reduce symptoms of anxiety and depression by restoring balance to the gut microbiome and improving neurotransmitter production.
▼
Chronic stress can negatively affect the gut microbiome, leading to dysbiosis and inflammation. Managing stress through practices like meditation supports gut health.
▼
Dietary changes like eating fiber-rich and fermented foods, managing stress, and engaging in regular physical activity can improve gut health and mental well-being.
Conclusion
As research continues to reveal the intricate connections between gut health and mental well-being, adopting strategies to promote a balanced gut microbiome may offer significant benefits for mental health. Paying attention to what we eat and actively managing our stress levels can contribute to a healthier gut and a happier mind.





